PTNS: Julianne’s Story
Meet Julianne

In 2023, Julianne’s family was making weekly trips to urgent care and doctor's offices. Julianne, a toddler at the time, was having severe, painful bladder spasms almost every day.
“I spent what felt like hours crying on the urgent care bathroom floor trying to get my 3-year-old to pee into a sample cup,” said Sophie, Julianne’s mom. They started taking cups home with them to be ready for the next trip. Any time they got in the car, Julianne would ask, “Are we going to Children’s Mercy?” The whole family was frustrated, frightened and losing sleep.
“We would be up in the middle of the night not knowing how to help her, because there was really nothing we could do,” said Sophie. “We were grateful that it wasn't a life-threatening issue, but when your child is in pain and there aren’t answers, it’s very scary.”
A long, frustrating road
Julianne, now 5 ½ years old, and her younger sister, Scarlett, 3 ½, were both born with vesicoureteral reflux, or kidney reflux. The condition causes urine to flow the wrong way, back up from the bladder into the kidneys. It can cause the bacteria from a urinary tract infection (UTI) to travel to the kidney and result in kidney infections.
Julianne had been on antibiotics to prevent infections since she was a baby, and she had successful surgery to correct the reflux in October 2023 at Children’s Mercy. But, outside of the reflux, Julianne continued to have painful bladder spasms.
“About a month after her surgery, we were in the ER,” said Sophie.
Julianne’s care team suspected that the bladder spasms had been going on so long that Julianne’s mind and body weren’t connecting when she tried to go to the bathroom now. She wasn’t getting rid of all her urine, which would then stagnate and cause another UTI and more pain.
“We did pelvic floor therapy and all of these things to try to fix the retention issue, and we weren’t having a ton of success,” said Sophie.
A new treatment option

“By that time, they were pretty frustrated,” said Azadeh Wickham, PhD, APRN, FNP-BC, Urology, who first met with Julianne and her family in August 2024. “I said, ‘I know you’ve been through it, but I have another trick up my sleeve.’”
PTNS, or Posterior Tibial Nerve Stimulation, uses low-voltage electrical stimulation to help block nerve messages that interfere with bladder function. Families appreciate that PTNS is non-invasive and non-pharmacological. But it does require time and consistency: The standard course is a 30-minute treatment every week for 12 weeks with maintenance sessions tailored to the patient’s needs after that.
Julianne started PTNS January 2025.
“They bring in a super small, portable device, and they find a spot right above the ankle bone on the inside of her leg,” explained Sophie. “They put a little acupuncture needle in, and it’s hooked up to the PTNS unit. They slowly increase it and ask, ‘Do you feel that?’ Then they go up to her comfort level. We just sit and hang.”
Patients don’t have to do anything during the session; most kids will play a game or watch a video to pass the time. Julianne likes to watch Sesame Street while she waits.
“It does buzz you; it’s a weird feeling,” said Dr. Wickham. “It’s not relaxing, but it’s not painful by any means.”
Unexpectedly swift results
Sophie said the family had low expectations after nearly 5 years of different interventions. But to their surprise, they were seeing positive results within 6 weeks: Julianne was having fewer bladder spasms and having an easier time going to the bathroom.
By the end of 12 weeks, Julianne was doing so well, they decided to try taking her off antibiotics. For the first time since she was 1 ½ years old, she’s been able to stay infection-free without medication.
“She has been medicine-free since March of this year and has been doing really well,” said Sophie. “It’s a night-and-day difference from where we were 2 years ago.”
Julianne is now going in for maintenance PTNS sessions every 3 months, and her care team will continue to monitor her progress and PTNS needs.
Something else to offer
Dr. Wickham started the PTNS program at Children’s Mercy in late 2020. She brought the therapy to her team’s attention after seeing new pediatric research on how PTNS can help the 1 in 10 kids who deal with urinary incontinence, frequency, urgency and/or UTIs.
“The reason I started this program is because of patients like Julianne and her family,” said Dr. Wickham. “They tried everything, and I wanted to have something else to offer.”
That “something else” has become a life-changing answer for quite a few Children’s Mercy families. And PTNS’s reputation has spread in the past 5 years as well.
Insurance companies are more likely to approve the third-line therapy now, increasing access to the treatments. Throughout the country, more organizations are offering PTNS, but Children’s Mercy is still the only pediatric hospital in the region with a program. Dr. Wickham lets families know PTNS is in their toolbox, even if they aren’t ready to try it yet.
“We’ve been having these conversations quite a bit earlier now,” said Dr. Wickham. “We’re trying to avoid families getting to the end of their ropes. That’s not a good feeling.”
They are taking that proactive mindset with Julianne’s younger sister. Scarlett’s experiences with kidney reflux have been much milder than Julianne’s, so far. Scarlett had her corrective surgery this fall and hasn’t had the retention issues Julianne had. She’s still on antibiotics and bladder spasm medication but will start weaning off meds over the coming months. They have a plan for PTNS if she starts having more trouble.
“Fingers crossed that we won’t have to have her do PTNS, but I’m really grateful we have that in our back pocket,” said Sophie.
Absolutely thriving

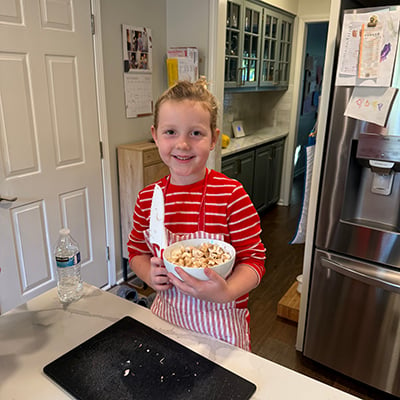
These days, Julianne just gets to be a kid. She's in kindergarten and loves music, playing outside and reading books. For her very limited screentime, she’ll always ask for a cooking show, and her family likes watching her recreate the episodes in her play kitchen.
“She’s doing great; she’s absolutely thriving now,” said Sophie. “She has always taken it in stride, goes with the flow and doesn’t complain. We’re just so proud of her and we love her to pieces.”
“Julianne's family is amazing; they’re such great partners in care,” said Dr. Wickham. “Julianne is a joy to take care of, and the whole family is just wonderful.”
Sophie recently attended a national conference with Dr. Wickham to share her family’s experience with PTNS. “These issues are more common than you might realize,” said Sophie, who advises other parents to keep pushing and find a provider who will keep looking for answers with you. “I never stopped pushing for what’s next. I’m so thankful Azadeh took us under her wing and told us, ‘We’re not giving up.’”